Pathology infographic: Breast Cancer-Related Lymphedema (BCRL)
Purpose
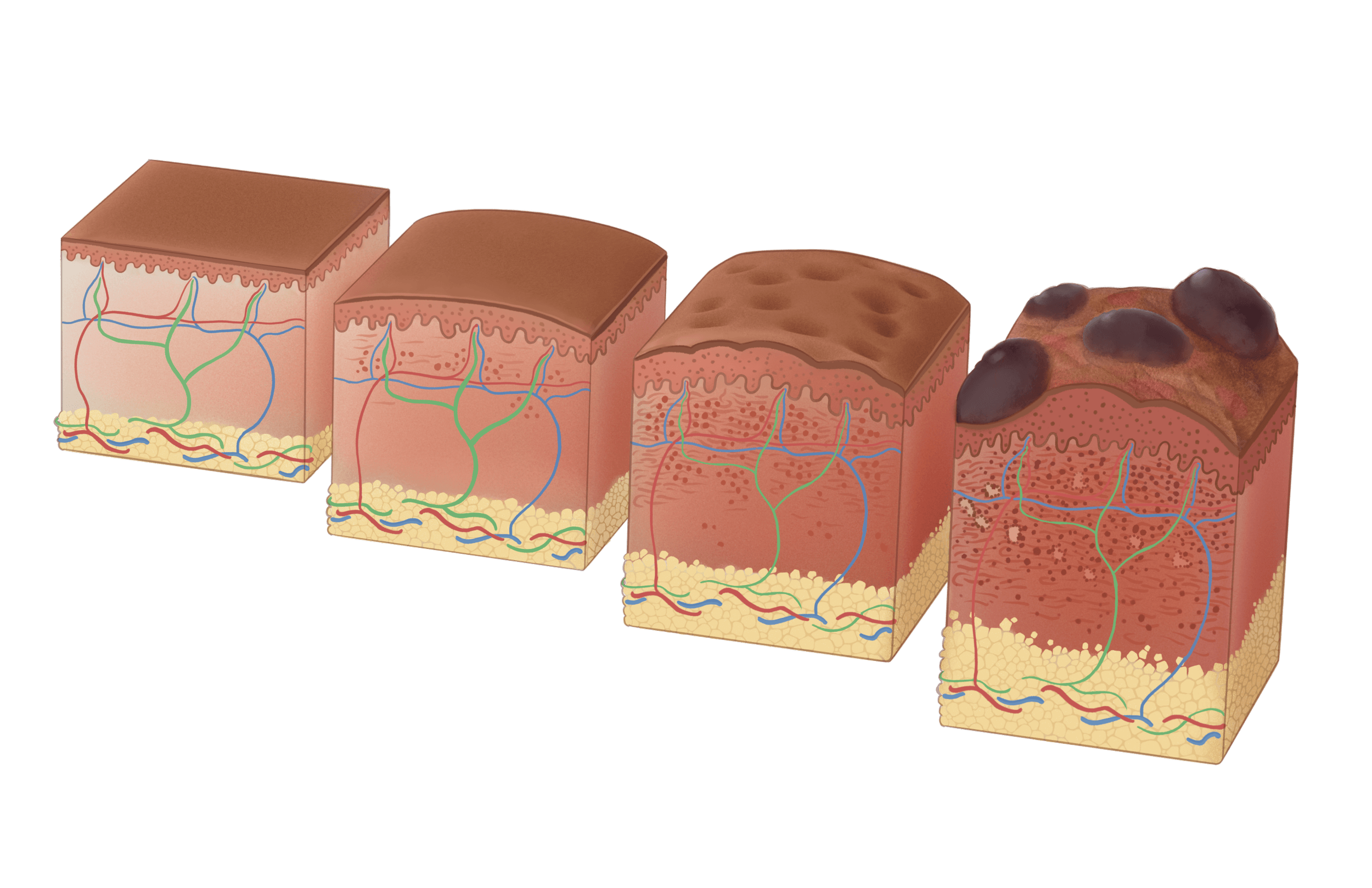
Breast Cancer Related Lymphedema (BCRL) affects up to one in five breast cancer survivors. Better awareness of this disease can help with prevention, identification, and treatment of this disease. The main goal of this infographic was to explain the pathology of this disease and visualize its progression.
Audience
Healthcare providers
Intended format
Healthcare printout or social media
Tools used
Procreate, Daz3D, Autodesk Maya, Adobe Photoshop, Adobe Illustrator
Client
David Mazierski, University of Toronto
Layout considerations
BCRL usually manifested in the arm due to disruption of the axillary lymph nodes. I decided to use the length of the arm to show the linear progression of the disease.
3D Maquettes
Daz 3D was used for posing and shading cues for the figure drawing, while Maya was used to create maquettes for the lymph nodes and tissue cubes. After adjustments in Photoshop, Final details were illustrated in Procreate.
Detail
Pathology textbooks, journal articles, and healthcare training materials were used to research the pathology of BCRL, in order to identify and visualize the progression of the disease at a histological and morphological level.
Academic references
Agur, A. M. R. (2019). Moore’s Essential Clinical Anatomy (6th ed.). LWW. https://www.biblio.com/book/moores-essential-clinical-anatomy-agur-bsc/d/1561536985
Anatomy of the Lymphatic System. (n.d.). Retrieved January 14, 2025, from https://www.brainkart.com/article/Anatomy-of-the-Lymphatic-System_21896/
Arkansas Lymphedema Therapy – The only nationally certified Lymphedema clinic in Arkansas. (n.d.). Retrieved January 14, 2025, from https://arlymphedematherapy.com/
Black, D. M., Jiang, J., Kuerer, H. M., Buchholz, T. A., & Smith, B. D. (2014). Racial Disparities in Adoption of Axillary Sentinel Lymph Node Biopsy and Lymphedema Risk in Women With Breast Cancer. JAMA Surgery, 149(8), 788–796. https://doi.org/10.1001/jamasurg.2014.23
Brian MacPherson Anne Gilroy, L. R. (2008). Atlas Of Anatomy (1st edition). Thieme Medical Publishers.
Byeon, J., Kang, E., Jung, J.-J., Cheun, J.-H., Seo, K. S., Kim, H.-K., Lee, H.-B., Han, W., & Moon, H.-G. (2024). Risk of Lymphedema After Sentinel Node Biopsy in Patients With Breast Cancer. Journal of Breast Cancer, 27(5), 323–333. https://doi.org/10.4048/jbc.2024.0180
Daneshgaran, G., Lo, A., Paik, C., Cooper, M., Sung, C., Jiao, W., Park, S., Ni, P., Yu, R., Vorobyova, I., Jashashvili, T., Hong, Y.-K., Kim, G., Conti, P., Chai, Y., & Wong, A. (2019). A Pre-clinical Animal Model of Secondary Head and Neck Lymphedema. Scientific Reports, 9, 18264. https://doi.org/10.1038/s41598-019-54201-2
Gebruers, N., Verbelen, H., De Vrieze, T., Coeck, D., & Tjalma, W. (2015). Incidence and Time Path of Lymphedema in Sentinel Node Negative Breast Cancer Patients: A Systematic Review. Archives of Physical Medicine and Rehabilitation, 96(6), 1131–1139. https://doi.org/10.1016/j.apmr.2015.01.014
Gillespie, T. C., Sayegh, H. E., Brunelle, C. L., Daniell, K. M., & Taghian, A. G. (2018). Breast cancer-related lymphedema: Risk factors, precautionary measures, and treatments. Gland Surgery, 7(4), Article 4. https://doi.org/10.21037/gs.2017.11.04
Grada, A. A., & Phillips, T. J. (2017). Lymphedema: Pathophysiology and clinical manifestations. Journal of the American Academy of Dermatology, 77(6), 1009–1020. https://doi.org/10.1016/j.jaad.2017.03.022
International Society of Lymphology. (2013). The diagnosis and treatment of peripheral lymphedema: 2013 Consensus Document of the International Society of Lymphology. Lymphology, 46(1), 1–11.
Jen. (2019a, November 24). Lymphedema Condition Overview [Causes, Stages, Symptoms, Treatments, Precautions]. Lymphedema Lifeline. https://lymphedemalifeline.org/articles/lymphedema/
Jen. (2019b, November 24). Lymphedema Condition Overview [Causes, Stages, Symptoms, Treatments, Precautions]. Lymphedema Lifeline. https://lymphedemalifeline.org/articles/lymphedema/
Kim, H.-K., Ju, Y. W., Lee, J. W., Kim, K.-E., Jung, J., Kim, Y., Lee, H.-B., Moon, H.-G., Noh, D.-Y., Seo, K. S., & Han, W. (2021). Association between Number of Retrieved Sentinel Lymph Nodes and Breast Cancer-related Lymphedema. Journal of Breast Cancer, 24(1), 63–74. https://doi.org/10.4048/jbc.2021.24.e9
Lin, S., Kim, J., Lee, M.-J., Roche, L., Yang, N., Tsao, P., & Rockson, S. (2012). Prospective Transcriptomic Pathway Analysis of Human Lymphatic Vascular Insufficiency: Identification and Validation of a Circulating Biomarker Panel. PloS One, 7, e52021. https://doi.org/10.1371/journal.pone.0052021
Liu, Z., Li, J., Bian, Y., Zhang, X., Cai, X., & Zheng, Y. (2023). Low-intensity pulsed ultrasound reduces lymphedema by regulating macrophage polarization and enhancing microcirculation. Frontiers in Bioengineering and Biotechnology, 11. https://doi.org/10.3389/fbioe.2023.1173169
Mestak, O., Mestak, J., Bohac, M., Edriss, A., & Sukop, A. (2013). Breast Reconstruction after a Bilateral Mastectomy Using the BRAVA Expansion System and Fat Grafting. Plastic and Reconstructive Surgery. Global Open, 1(8), e71. https://doi.org/10.1097/GOX.0000000000000022
Netter, F. H. (2022). Atlas of Human Anatomy: Latin Terminology: English and Latin Edition (7th edition). Elsevier Canada.
Norman, S. A., Localio, A. R., Potashnik, S. L., Simoes Torpey, H. A., Kallan, M. J., Weber, A. L., Miller, L. T., DeMichele, A., & Solin, L. J. (2009). Lymphedema in Breast Cancer Survivors: Incidence, Degree, Time Course, Treatment, and Symptoms. Journal of Clinical Oncology, 27(3), 390–397. https://doi.org/10.1200/JCO.2008.17.9291
Paskett, E. D. (2015). Symptoms: Lymphedema. In P. A. Ganz (Ed.), IMPROVING OUTCOMES FOR BREAST CANCER SURVIVORS: PERSPECTIVES ON RESEARCH CHALLENGES AND OPPORTUNITIES (Vol. 862, pp. 101–113). Springer-Verlag Berlin. https://doi.org/10.1007/978-3-319-16366-6_8
Publishing, L., & CVDTeam. (2009, September 9). Anatomical distribution of tissue fluid and lymph in soft tissues of lower limbs in obstructive lymphedema—Hints for physiotherapy. Servier - Phlebolymphology. https://www.phlebolymphology.org/anatomical-distribution-of-tissue-fluid-and-lymph-in-soft-tissues-of-lower-limbs-in-obstructive-lymphedema—hints-for-physiotherapy/
Sentinel Lymph Node Biopsy—NCI (nciglobal,ncienterprise). (2022, August 19). [cgvArticle]. https://www.cancer.gov/about-cancer/diagnosis-staging/staging/sentinel-node-biopsy-fact-sheet
Sharma, A., & Schwartz, R. A. (2012). Stewart-Treves syndrome: Pathogenesis and management. Journal of the American Academy of Dermatology, 67(6), 1342–1348. https://doi.org/10.1016/j.jaad.2012.04.028
Slide Library | Virtual Pathology at the University of Leeds. (n.d.-a). Retrieved January 15, 2025, from https://www.virtualpathology.leeds.ac.uk/slides/library/
Stages of Lymphedema in the Upper Limb | AMI Meeting 2020. (n.d.). Retrieved January 14, 2025, from https://meetingarchive.ami.org/2020/project/stages-of-lymphedema-in-the-upper-limb/
Willard-Mack, C. L. (2006). Normal Structure, Function, and Histology of Lymph Nodes. Toxicologic Pathology, 34(5), 409–424. https://doi.org/10.1080/01926230600867727
Wolf, S., von Atzigen, J., Kaiser, B., Grünherz, L., Kim, B.-S., Giovanoli, P., Lindenblatt, N., & Gousopoulos, E. (2022). Is Lymphedema a Systemic Disease? A Paired Molecular and Histological Analysis of the Affected and Unaffected Tissue in Lymphedema Patients. Biomolecules, 12(11), Article 11. https://doi.org/10.3390/biom12111667
Interested in working together? Let’s talk about it.
I take on projects big and small. Reach out and let’s talk details.